The COVID-19 pandemic caused unprecedented global devastation. WHO reports that there have been over 770 million confirmed cases of COVID-19 with almost 7 million deaths reported (as of September 13, 2023).
The development and distribution of COVID-19 vaccines were instrumental in lowering the risk of severe hospitalizations and deaths from COVID-19.
COVID-19 vaccines: the mRNA vaccine milestone
Development
During the pandemic, several types of COVID-19 vaccines were developed. Some vaccines had inactivated coronaviruses or isolated proteins from the virus to stimulate an immune response. This technique of making vaccines has been used for decades.
However, the biggest breakthrough in vaccine technology, in recent times, was the approval of mRNA-based vaccines for public use.
This condensed timeline for the COVID-19 vaccine approval was unprecedented. In the past, it could take decades for vaccines to go from research to commercial distribution. However, to deal with the rising body count from the SARS-CoV-2 virus and its strains, mRNA-based COVID-19 vaccines were authorized within a year of when the pandemic broke.
Once approved, the vaccine rollout took collaboration between countries, public health agencies, scientists, doctors, and many more for millions of global citizens to receive COVID-19 vaccinations.
Impact
The mass vaccination programs had a profound impact on reducing the severity of COVID-19 illness. While breakthrough infections can occur in vaccinated individuals, the vaccines significantly reduced the risk of severe disease, hospitalization, and death.
The scientists responsible for the research that paved the way for mRNA vaccines were recognized for their groundbreaking work. Katalin Karikó and Drew Weissman were awarded the 2023 Nobel Prize in Physiology or Medicine for their work on mRNA vaccines.
By vaccinating a large proportion of the population, mass vaccination programs minimize the burden on healthcare systems, so that resources can be directed to other critical medical needs.
Challenges
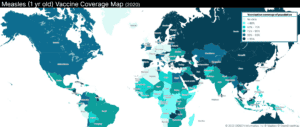
- Over 13 billion COVID-19 vaccine doses were administered worldwide, as of September 9, 2023. While this sounds like a high number, one-third of the global population unfortunately remains unvaccinated.
- There remains a level of distrust and vaccine hesitancy in pockets worldwide, which may need to be addressed.
- The level of vaccine misinformation during the pandemic has far-reaching consequences, beyond the COVID-19 vaccines. In April 2023, the United Nations Children’s Fund (UNICEF) reported that almost 67 million children were deprived of routine childhood vaccines during the pandemic and one of the reasons was mistrust in vaccines.
Future
Apart from saving lives during the COVID-19 pandemic and after, the approval of mRNA-based vaccines has incredible potential for other diseases. mRNA vaccines are being studied for use against other SARS viruses, hepatitis C, malaria, tuberculosis, other communicable diseases, and even some cancers.